Professor Xie Qing: Risk assessment and screening of HCC, an urgent problem in the management of chronic hepatitis B in the anti-virus era.
Original Ruijin Infectious Diseases Department Ruijin Infectious Diseases Department
At the 4th Yangtze River Delta Liver Disease Summit Forum and Multidisciplinary Symposium on Diagnosis and Treatment of Liver Tumors in 2020, Professor Xie Qing, Director of Infectious Diseases Department of Ruijin Hospital affiliated to Shanghai Jiaotong University School of Medicine, gave a wonderful report entitled "Risk Assessment and Screening of ——HCC, an urgent problem in the management of chronic hepatitis B in the anti-virus era". The following is a written record.
Professor Xie Qing first introduced a typical clinical case of hepatocellular carcinoma (HCC) after regular follow-up of antiviral therapy for chronic hepatitis B (CHB):
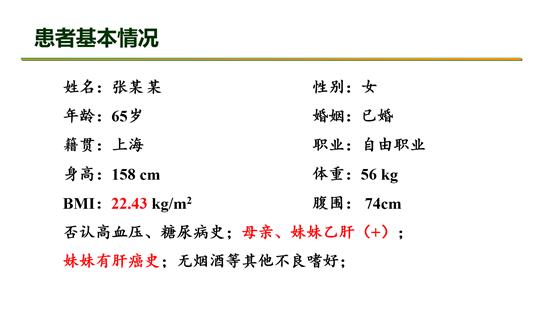
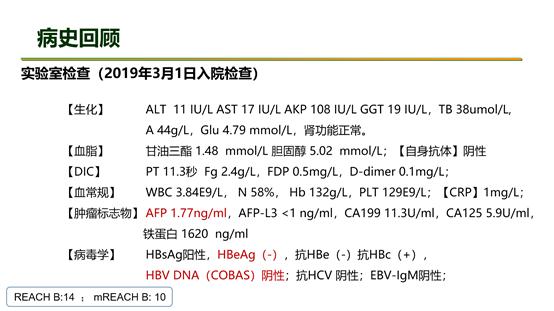
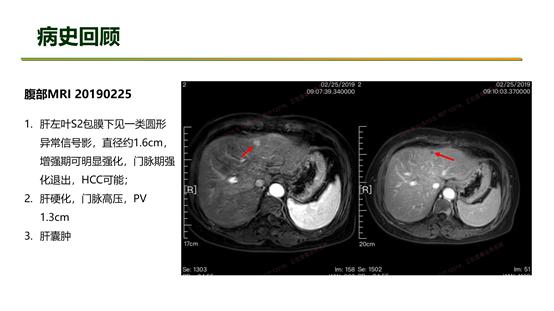
The patient is female, who has been diagnosed with hepatitis B for more than ten years, and her mother and sister have hepatitis B (+), and her sister has a history of hepatitis B liver cancer, and has no other chronic diseases and personal bad hobbies; Liver biopsy was performed after the patient had mild abnormal liver function for the first time, and the result of liver puncture showed that inflammation was grade 3 and fibrosis was grade 2 (G3S2), so entecavir was given antiviral treatment. Patients were followed up regularly for 3-6 months. During the 5-year follow-up of antiviral therapy, low-echo nodules in the left lobe of liver were found by B-ultrasound, with a diameter of about 1.5cm, and AFP was normal. After enhanced MRI and multidisciplinary consultation of liver tumors, HCC was diagnosed and surgically removed. Postoperative pathology showed that hepatocellular carcinoma was grade II-III, with a size of 1.5×1.3×0.6cm, MVI=0, and the surrounding liver tissue showed micronodular cirrhosis, G4S4.
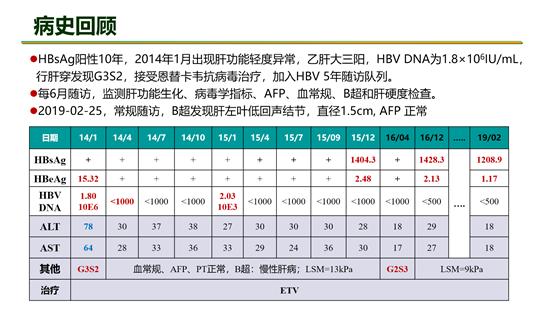
It can be seen from the above cases that after receiving antiviral treatment, patients with early cirrhosis can not completely avoid the risk of HCC even if they maintain high compliance and follow-up regularly to achieve sustained virological and biochemical response.
This brings severe challenges to the management of CHB patients: in the era of antiviral therapy, how should we accurately assess the risk of HCC and standardize HCC screening?
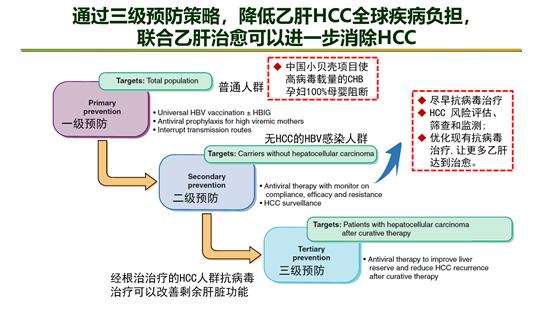
The incidence and mortality of HCC in China are high, ranking the top five in the list of high-incidence malignant tumors in China all the year round, and hepatitis B is the main cause of HCC in China. At present, the prevention and treatment of HCC mainly reduces the global disease burden of hepatitis B HCC through three-level prevention strategies, and combined with hepatitis B cure can further eliminate HCC. At the level of primary prevention, the introduction and implementation of the "small shell" project in China has made 100% of CHB pregnant women with high viral load blocked from mother to child; At the level of secondary prevention, through the management of HBV-infected people without HCC, they can receive antiviral treatment as soon as possible, and optimize the existing antiviral scheme to make more hepatitis B patients cure; At the level of tertiary prevention, the remaining liver function can be improved and the risk of HCC recurrence can be minimized by allowing the radical HCC population to continue antiviral treatment.
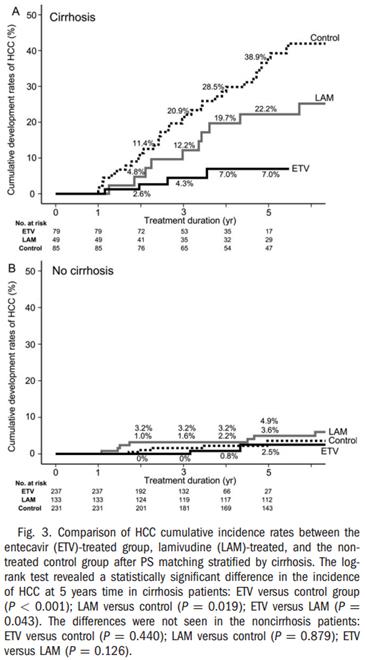
A large number of clinical studies have shown that long-term oral administration of NAs antiviral drugs can reduce the risk of HCC, but it cannot completely prevent HCC. The following are data from Japanese and Hong Kong, China population cohorts.
Japanese data:
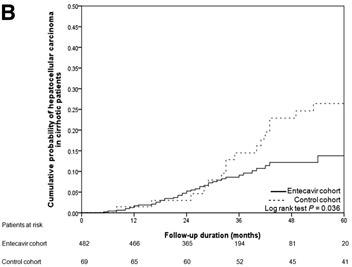
Hong Kong, China data:
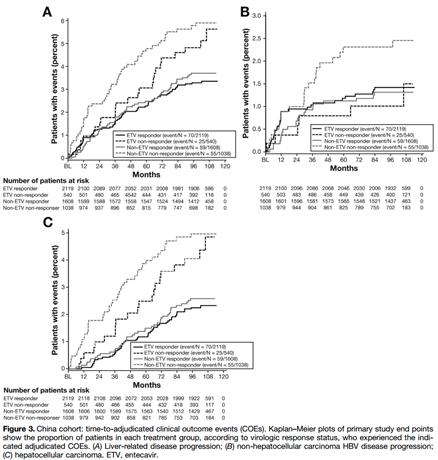
A clinical study from 24 countries shows that obtaining virological response can reduce the progression of liver-related diseases and the incidence of HCC, but there is still a risk of HCC. The research results were published in Clin Gastroenterol Hepatol this year (if = 8.549), and the team of Ruijin Hospital provided nearly 150 cases with a 10-year follow-up cohort.
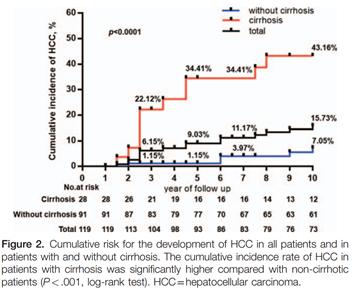
A 10-year cohort study of Jia Jidong’s team in China showed that the effective inhibition of virus by NAs can significantly reduce the occurrence of HCC, but there is still a high risk of HCC in patients with existing liver cirrhosis, and the cumulative incidence of HCC can be as high as 43.16%.
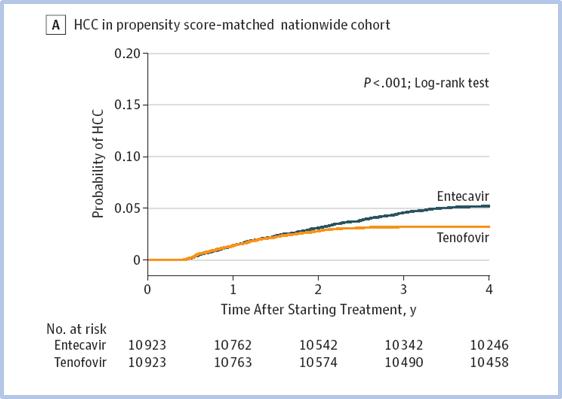
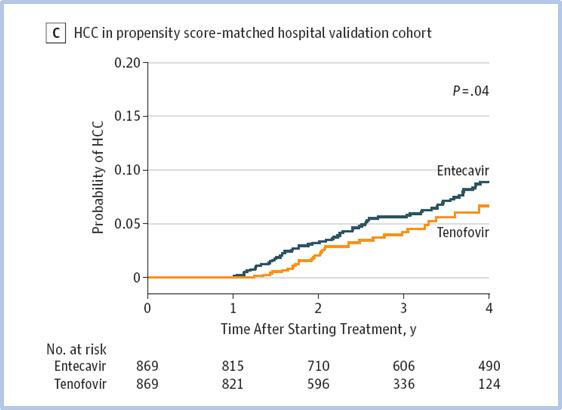
A nationwide historical cohort study in Korea also aims to explore the risk of HCC in CHB patients receiving antiviral therapy. A total of 24,156 adult CHB patients with newly diagnosed NA were included in the study, and they were treated with ETV (n = 11,464) or TDF (n = 12,692), among which 26.1% and 27.5% were cirrhosis patients in ETV group and TDF group respectively. At the same time, the hospital cohort was used for external verification, including 1560 newly diagnosed adult CHB patients treated with ETV and 1141 patients treated with TDF. The results are as follows.
Xie Qing’s team’s evidence proves that antiviral therapy can reduce the occurrence of HCC, but there is still the risk of HCC after NAs treatment, and PegIFN treatment of CHB is better than NAs (especially for high-risk people) in reducing the risk of HCC. This retrospective study used the published HCC risk scoring system to score each patient, with an average follow-up time of 5.41 years.
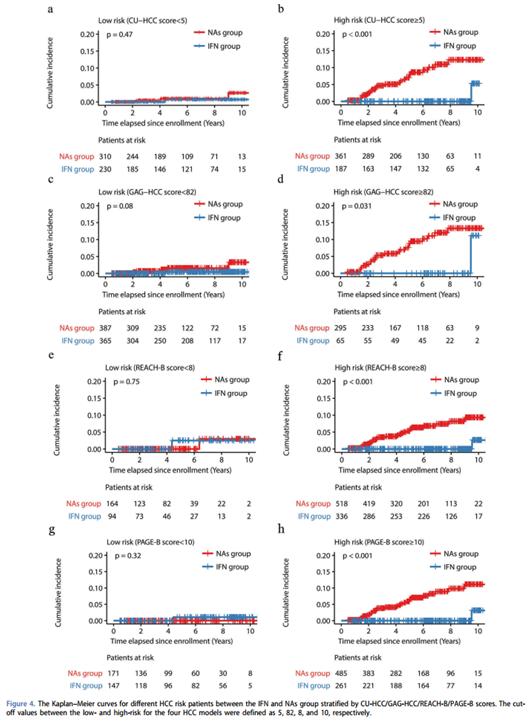
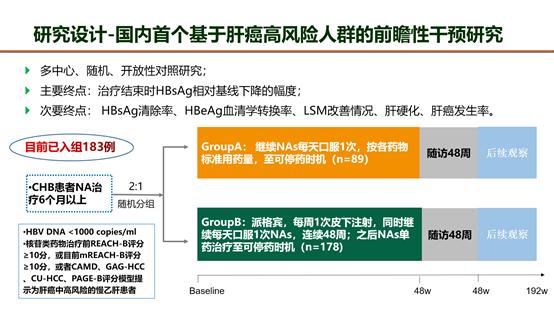
Combined with the above clinical research ideas, Ruijin Hospital team has carried out the first prospective intervention study based on high-risk population of HCC in China, which was randomly divided into NAs treatment group and IFN+NAs combination treatment group. The primary/secondary endpoints and research outline are briefly described as follows.
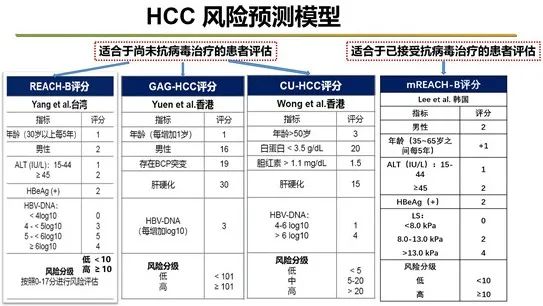
A large number of research data show that antiviral therapy can not completely prevent HCC, so the risk assessment of HCC during HBV infection has become an important proposition. The existing HCC risk prediction models include the evaluation model for patients who have not received antiviral treatment, represented by REACH-B score (Taiwan, China), GAG-HCC score (Hong Kong, China) and CU-HCC score (Hong Kong, China), and the evaluation model for patients who have received antiviral treatment, represented by mREACH-B score (Korea).
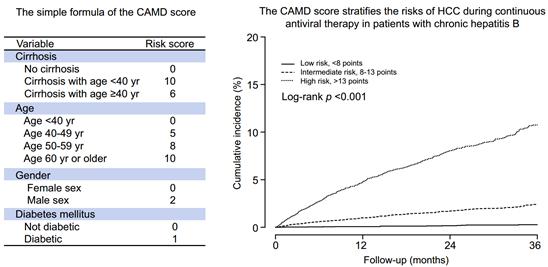
CAMD scoring adds diabetes as the basic disease to the traditional scoring rules, which optimizes the application of HCC risk prediction model in high-risk patients.
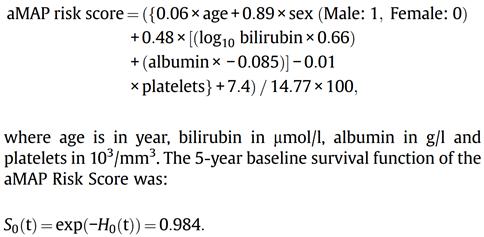
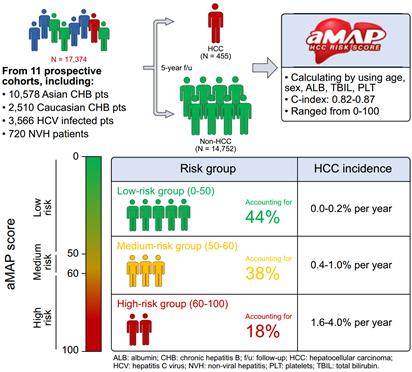
The latest aMAP score is combined with the patient’s age, sex, bilirubin, albumin, platelet and other indicators to optimize the operation model. The aMAP score of 0-50 is defined as a low-risk group of HCC, and the cumulative incidence of HCC in 5 years is 0.8%. Correspondingly, the score of 50-60 is defined as a medium-risk group, and the cumulative incidence of HCC in 5 years is 4.2%, while the score of 60-100 is defined as a high-risk group.
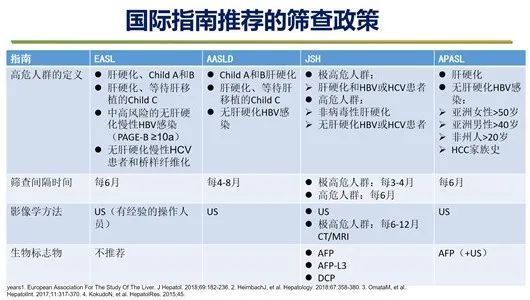
At present, the HCC screening policies recommended by major international guidelines in the field of hepatology are not the same. Here, Professor Xie Qing makes a clear comb for the participants.

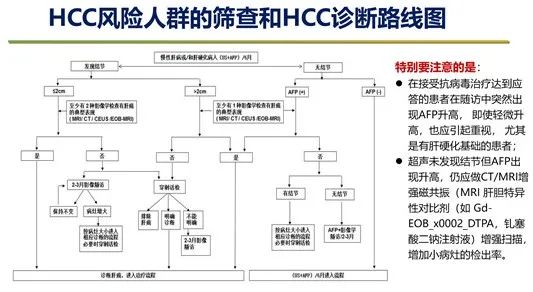
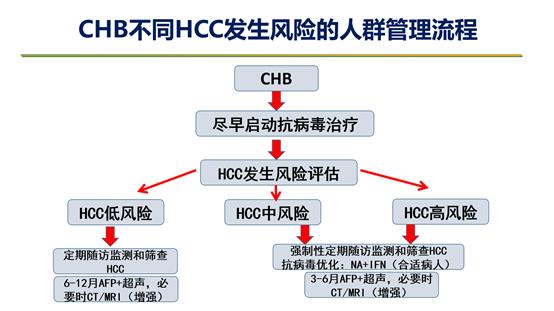
Finally, Professor Xie Qing summarized the diagnosis route of HCC and the crowd management process of different risks of HCC in CHB, based on the major clinical research results, guidelines recommendation and clinical experience at home and abroad, so as to provide reference for clinicians to further guide clinical practice.
Read the original text